
CASE SUMMARY
A 75-year-old female was referred to the Bochner Eye Institute for cataract surgery evaluation. Her best-corrected visual acuity was 20/100 OD (-2.00 -1.00 x 180) and 20/80 OS (-1.75 -1.00 x 175). She was in good general health with no contraindications to surgery. Ocular examination revealed bilateral cataracts with 3+ nuclear sclerosis and 2+ cortical changes. Fundus exam and OCT of the macula were normal. Corneal topography showed no irregular astigmatism.
After discussing the risks and benefits, the patient consented to bilateral cataract surgery. She underwent femtosecond laser-assisted phacoemulsification with toric IOL implantation. A mini-monovision strategy was employed: targeting emmetropia in the dominant right eye and -1.25 D in the left eye for near vision.
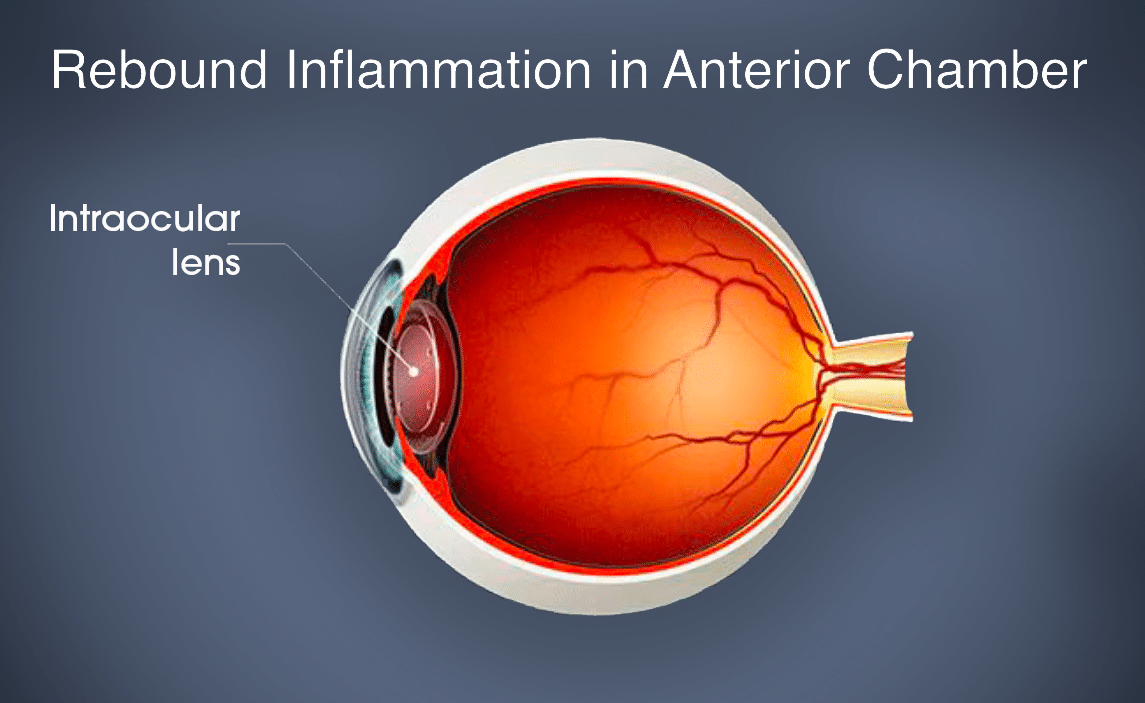
The immediate postoperative course was uneventful. However, two weeks after completing a tapering course of topical steroids, she presented with bilateral eye discomfort, photophobia, and redness. Clinical examination revealed rebound anterior uveitis, with 1+ to 2+ anterior chamber cells in both eyes. The corneas remained clear, and the IOLs were well-positioned.
POST-OPERATIVE TREATMENT:
Topical Pred Forte was reintroduced at a frequency of four times daily for two weeks, followed by a tapering schedule:
- three times daily for two weeks
- twice daily for two weeks
- once daily for one week
Follow-up evaluations at 3 and 6 weeks demonstrated a gradual resolution of inflammation and improvement in symptoms. Upon completion of the taper, she remained symptom-free with no evidence of rebound inflammation.

KEY LEARNING POINTS:
Rebound inflammation, or rebound iritis, is a recurrence of eye inflammation following cataract surgery, typically emerging during the tapering of postoperative steroid medications. This condition is characterized by the presence of white blood celks (leukocytes) in the anterior chamber of the eye and can lead to symptoms such as eye redness, pain, blurred vision, and photophobia.
1. CAUSES AND RISK FACTORS:
- Incomplete Inflammation Control: Premature tapering or discontinuation of anti-inflammatory medications can result in residual inflammation.
- Residual Lens Material: Leftover lens fragments in the anterior chamber or behind the iris may incite an inflammatory response. It is important to look for a lens fragment especially in the inferior angle. Nuclear fragments will need removal. Cortical remnants will typically resolve with time and the use of steroid drops.
- Patient Non-Compliance: Improper adherence to prescribed postoperative medication regimens can contribute to rebound inflammation
- Other Risk Factors: Patients with African American descent, diabetics, or those requiring pupil expansion devices during surgery have a higher risk of prolonged postoperative inflammation.
- Chronic Endophthalmitis: A less common but serious condition characterized by recurrent episodes of inflammation and decreased vision. It typically presents with milder symptoms than acute endophthalmitis but requires prompt diagnosis and treatment to prevent vision loss.
2. MANAGEMENT STRATEGIES:
- Reinitiation of Steroid Therapy: Resuming topical corticosteroids, such as prednisolone acetate 1%, with a gradual tapering schedule can help control inflammation.
- Cycloplegic Agents: In severe cases, medications like cyclogel 1% or homatropine 5% may be used to prevent the formation of synechiae and alleviate ciliary body spasm, reducing pain.
- Patient Education: Emphasizing the importance of adhering to medication schedules and proper administration techniques is crucial.
- Follow-Up Care: Regular monitoring allows for timely adjustments to treatment plans and ensures resolution of inflammation.
FINAL THOUGHTS:
Early recognition and appropriate management of rebound inflammation are essential to prevent complications and preserve visual function after cataract surgery.
Recurrent inflammation following cataract surgery, though relatively uncommon, can present significant challenges. Understanding its causes, risk factors, and management strategies is crucial for optimal patient outcomes.Close monitoring and patient education are vital components of effective postoperative care.
CLICK HERE to read additional articles on persistent iritis.


